Exclusion Criteria for Outpatient Management
- Social Circumstances
- Pregnant (NEEDS D/W Obstetrics and Gynaecology)
- High Risk Bleeding
- Possible PE with high PESI score (calculate PESI / sPESI – on MDCalc)
- Immobility/Severe Pain
- Severe Uncontrolled Hypertension
- Recent GI/Intracranial Bleed or other significant bleed / bleeding risk
- Renal Failure requiring IV heparin (eGFR<30) or renal dosing treatment dose dalteparin
http://intranet/resource.asp?uid=38637
- Significant co-morbid disease requiring admission (COPD, cardiac failure, active alcohol/drug use)
- Iliofemoral thrombosis (consider discussion with vascular surgery)
Management in iv drug users:
Cellulitis or injection site abscess - Admit for IV antibiotics +/- Incision/Drainage
Chaotic Lifestyle – High chance DNA for scan
Doppler USS Leg
| NEGATIVE |
POSITIVE |
If D-Dimer positive without any other possible cause: Discharge home, and review in 1 week for possible repeat Doppler ultrasound. Decide on interim anticoagulation case by case.
If D-Dimer result negative: DVT unlikely, consider alternative diagnosis and discharge. |
Start apixaban if no
contraindications.
Consider edoxaban (after 5 days treatment dose
dalteparin) if medication
compliance a concern. |
If DVT unlikely, consider and treat the following diagnosis accordingly
| Alternative Diagnosis |
Treatment Pathway |
|
Baker’s Cyst
|
Refer back to GP, consider physiotherapy
|
|
Cellulitis
|
Follow Cellulitis pathway
|
|
Superficial Thrombophlebitis
|
Treat as Superficial Thrombophlebitis
|
|
Musculoskeletal
|
Consider orthopaedics if indicated
|
|
Arterial Insufficiency
|
Consider vascular referral if indicated
|
|
Other
|
(specify and treat accordingly)
|
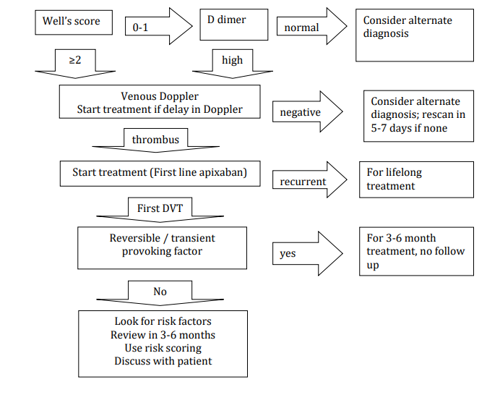
1st Line Treatment: Apixaban:
First choice of treatment of first presentation of VTE, and prevention of recurrent VTE
Dosing: 10mg BD daily for 7 days followed by 5mg BD. For Long Term Anticoagulation > 12 months: 2.5mg BD Apixaban after completed 6 months of treatment dose.
Calculate Creatinine clearance. No dose adjustment for mild to moderate renal impairment. If severe renal impairment (CrCl 15-29ml/min) use with caution d/w pharmacy or senior physician. Not recommended for patients on dialysis or creatinine clearance <15ml/min, use IV heparin or renal dosing treatment dose dalteparin and warfarin for this group (D/w renal team).
Contraindicated in patients receiving strong inhibitors of both CYP3A4 and P-gp, such as: azole-antimycotics (eg ketoconazole, itraconazole, voriconazole and posiconazole);
HIV protease inhibitors (eg Ritonavir).
Contraindicated in patients receiving strong inducers of both CYP3A4 and P-gp, such as rifampicin, phenytoin, carbamazepine, phenobarbital, St. John’s Wort.
Caution should be exercised if considering combined use with NSAIDs or anti-platelets, and in renal and hepatic impairment (discuss with pharmacy and senior medical staff.)
The BGH pharmacy will issue a supply at discharge, GP surgeries will issue prescriptions for remainder of the treatment course. Patients should be counselled and information leaflet supplied – pharmacy on AAU will assist with this
Consider LMWH
If alcohol/drug user: Ascertain risk, i.e., likelihood of continual IVDA, chaotic lifestyle, not registered with GP, and d/w senior. If not suitable for apixaban, consider once daily edoxaban (after 5 days treatment dose dalteparin) or daily SC treatment dose dalteparin. Platelets to be checked after 5/7 of therapy.
Oncology patients: Liaise with oncology to discuss commencing treatment with apixaban, preferred for treatment of VTE in the majority of patients with cancer, with treatment dose dalteparin an alternative treatment option.
Supportive measures
Compression Stockings: No evidence for compression stockings to prevent
postthrombotic syndrome so routine use is not recommended. In select patients it may
provide symptomatic relief.
Exercises: Ensure patient given advice on exercises and elevation (Gentle walking for 6
weeks, lower leg exercises, leg elevated when resting)
Education: Give patient DVT information booklet and advise to seek medical attention
if symptoms of PE or worsening leg symptoms. Discourage travel by air/long distance
for 2/52 post diagnosis.
Discharge: Use \vte template for discharge letter
Severe DVT:
Severe pain, swelling and discolouration of the leg suggestive of phlegmasia cerulea dolens, inferior vena cava thrombosis or extensive iliofemoral thrombosis with < 14 days symptoms. Discuss such cases with Vascular Surgery regarding further intervention
Long term management of confirmed DVT
Look for provoking and risk factors
- Active cancer –CXR, breast examination, history and exam to exclude
undiagnosed malignancy, PSA and urinalysis, check if females are up to
date with cervical screening, other imaging on case to case basis – discuss
with senior
- Medical hospitalisation > 4 days within 2 months
- Recent trauma (lower extremity or severe trauma)
- Major surgery within 3 months
- Pregnancy – needs Obstetrics involvement
- Thrombophilia – screening only warranted in young people
- Medical comorbidities: e.g. haematological diseases, nephrotic syndrome,
autoimmune diseases etc.
- Medications including : oestrogen containing oral contraceptives, tamoxifen,
raloxifene, thalidomide, pomalidomide, lenalidomide, HRT
- Smoking – advise on smoking cessation
- Obesity – advise on weight loss
- Recent long distance air travel
- Prolonged immobilisation of any cause
- Strong family history
Follow up
At present there is no DVT follow up clinic in NHS borders.
Patients with provoked DVT – define treatment length in discharge letter, no need for routine hospital follow up
Patients with PE – refer to respiratory clinic for follow up. If unprovoked, book screening tests for potential provoking factors.
Patients with unprovoked DVT – if not for lifelong anticoagulation straightaway then follow up in ACU between 4-6 months. Discuss stopping anticoagulation 1 month prior with patient if D dimer needed for risk assessment score. Discuss risks of this with patient initially if possible – if high risk anyway then decide for lifelong anticoagulation early. Book screening tests for potential provoking factors.
Possible risk assessment approaches for unprovoked DVT (risks / benefits need discussion with patient):