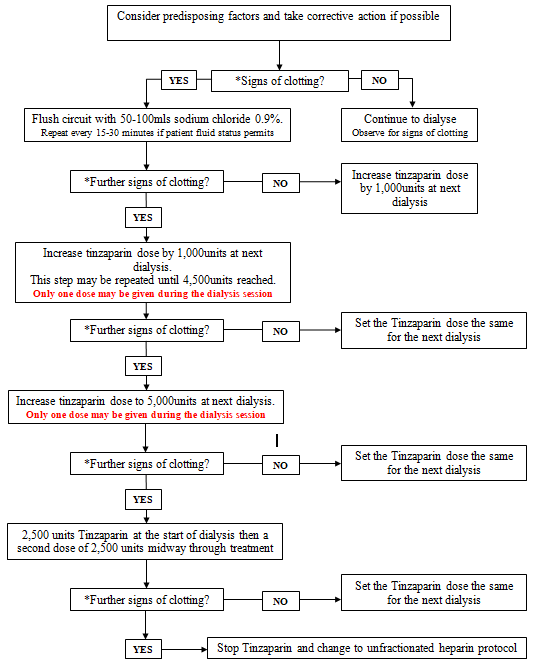
Tinzaparin is the preferred LMWH for use in haemodialysis circuits. Dose finding studies in haemodialysis patients have shown that short term and long term use of tinzaparin is safe in this group (2-4).
The anticoagulant effect of unfractionated heparin can be predictably reversed by the administration of protamine sulfate in the event of serious bleeding. While protamine is less effective at reversing the effect of LMWHs, tinzaparin is the LMWH preparation most amenable to reversal by protamine with a neutralisation effect of 86% reported (5).
Intravenous administration of tinzaparin or unfractionated heparin should always be in accordance with a valid prescription and the dose confirmed independently by 2 registered nurses. Concurrent anticoagulation must be taken into consideration. If the patient has received a dose of tinzaparin then no unfractionated heparin may be given.
Heparin Induced Thrombocytopaenia
Rarely, patients may be diagnosed with type II heparin-induced thrombocytopenia (HIT). This is a result of antibody formation to the heparin-platelet factor 4 complex which leads to a decline in platelet count and, more importantly, is associated with a risk of venous and arterial thrombosis.
The recommended local policy is to use Argatroban. This is a direct thrombin inhibitor, has a short half-life (45 minutes) and has hepatic clearance. It is therefore the drug of choice if invasive procedures are planned or in patients with renal impairment. Contact the renal consultants or renal pharmacist (bleep 2025) for advice.
Dialysis without anticoagulation
Where the dialysis session is less than 3 hours duration no tinzaparin may be given and heparin free dialysis should be considered.
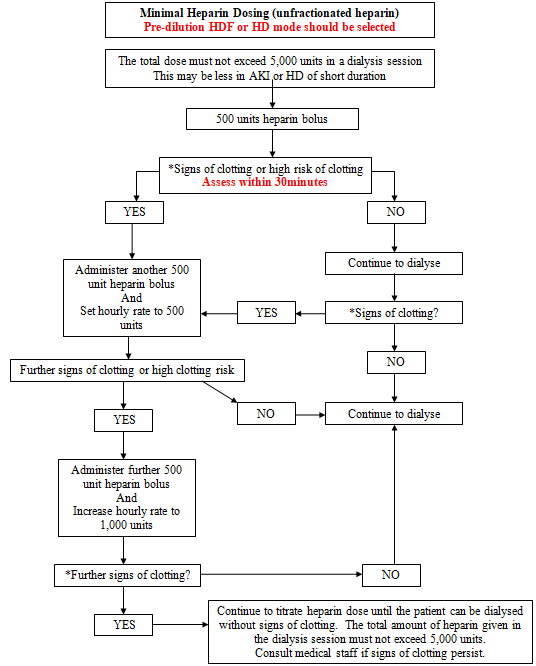
Clotting in the dialysis circuit
Factors that may contribute to clotting in the extracorporeal circuit may include:
- Intermittent blood flow. Maintain the blood flow at the optimum rate. Adjust dialysis access if necessary.
- High haemoglobin levels may increase clotting risk. Also, additional precaution is advised if the patients haemoglobin is low and there is a risk of losing the blood lines due to clotting
- Administration of blood transfusion during dialysis.
- High UF rates.
- Large reduction in relative blood volume (RBV reading).
- Haemodiafiltration in post dilution mode. Pre dilution mode or standard HD should be set whenever there is increased risk of clotting.
- Dialysis without any anticoagulant.
Signs of blood clotting in the extracorporeal circuit may include:
- Extremely dark blood.
- Shadows or streaks in dialyser. The circuit may be flushed with 100mls of sodium chloride 0.9% to allow suspected streaks to be seen more easily.
- Visible clots in venous chamber or rising venous pressure.
- Rapid filling of transducers.
- Presence of clots at arterial side of dialyser head.
- Rising transmembrane pressure (TMP).
- High system pressure alarm.
Concurrent anticoagulation
Some dialysis patients may be on concurrent full dose or prophylactic dose anticoagulation with warfarin, unfractionated heparin or low molecular weight heparin. Anticoagulation for dialysis in these patients should be as follows:
Concurrent anticoagulation | Anticoagulation strategy for dialysis |
Treatment dose warfarin with INR > 2 | Heparin free dialysis or unfractionated heparin protocol if evidence of clotting or previous clotting |
Continuous intravenous unfractionated heparin | Heparin free dialysis or unfractionated heparin protocol if evidence of clotting or previous clotting |
Treatment dose low molecular weight heparin | Heparin free dialysis or unfractionated heparin protocol if evidence of clotting or previous clotting |
Enoxaparin 20mg as venous thromboembolism prophylaxis | Administration of enoxaparin at 2200 hrs. Usual tinzaparin schedule on dialysis |
Intermittent subcutaneous unfractionated heparin (Minihep) | Heparin free dialysis or unfractionated heparin protocol if evidence of clotting or previous clotting |