-
Children with epidural infusions may only be nursed on designated wards and be cared for by registered nurses who:
- holds a valid current (3 yearly) certificate of attendance of the Acute Pain Service epidural lecture.
- declares her/himself to be competent -
If an opiate has been added to the epidural local anaesthetic infusion then no other opioids should be given whilst epidural infusion is in progress.
-
All patients who have an epidural infusion should have a patent IV cannula in case of adverse reactions
-
If epidural opiates are being used, naloxone should be readily available on the ward and registered nurses should know where it is located
Monitoring epidural infusions
- Pulse, Respiratory rate, Oxygen Saturations and Sedation score should be recorded on the PEWS chart:
In recovery: every 15 mins
On ward: 1/2 hourly for first 1 hour
Hourly thereafter until; the epidural is discontinued
If the child receives a “top-up” of levobupivacaine stronger that 0.125%, the patient must have their BP recorded every 5 minutes for 30 minutes. - Motor score must be recorded on the epidural chart:
In recovery: before returning to the ward
On ward: 1/2 hourly for 2 hours
4 hourly thereafter - Sensory level must be recorded on the epidural chart:.
In recovery: on anaesthetist’s instruction and before transfer to the ward.
On ward: 6hourly and if any of the following are noted:- inadequate pain relief
- hypotension
- increased motor block
- nausea and vomiting
- before restarting the epidural infusion if it was stopped due to high sensory level
- one hour after any increase in the epidural infusion.
- Temperature should be recorded on the PEWS chart every 4 hours or more frequently depending on the child’s condition.
- Pump Recordings must be recorded on the epidural chart as per hospital policy, ensuring that the amount delivered and the amount remaining add up to the original starting total.
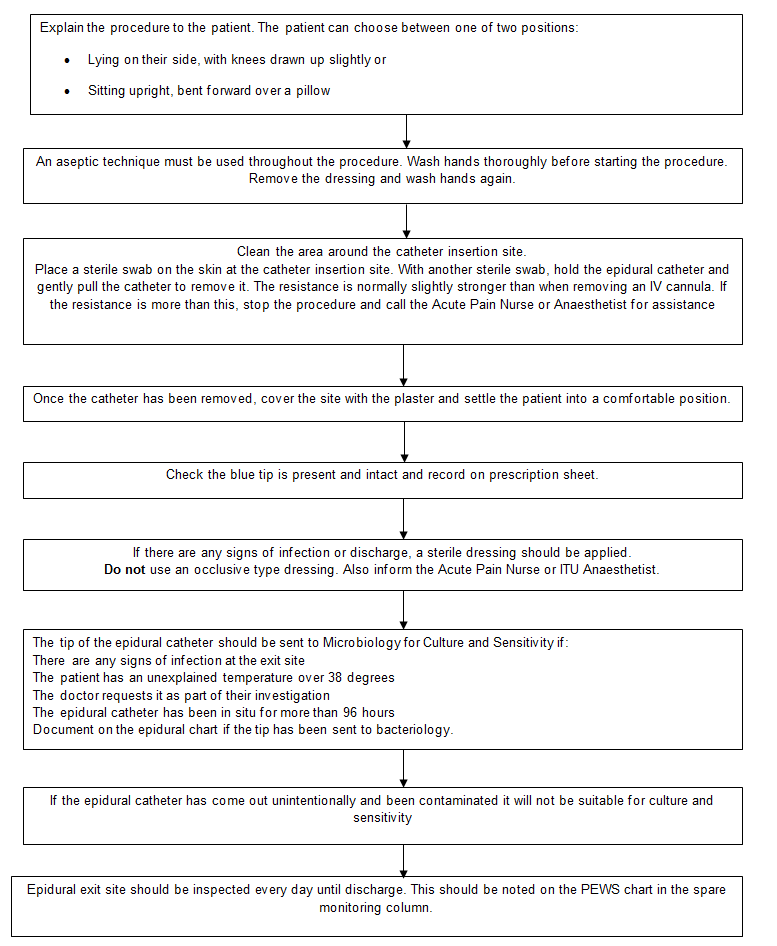
- Epidural Exit Site: While the epidural infusion is in progress, the exit must be checked on every shift for signs of leakage or infection. Once the epidural catheter has been removed, the exit site must be checked daily until the patient is discharged from hospital. This must be documented on the PEWS chart. Any signs of infection must be reported to the Acute Pain Team or On Call/Duty anaesthetist.
- Temperature must be recorded on the PEWS chart every 4 hours (or more frequently, if the patients condition requires it)
- Pump recordings must be recorded on the epidural chart as per Hospital policy, ensuring that the 'amount delivered' and the 'amount remaining' add up to the original starting total.
Measuring sensory levels
How to perform the sensory level measurement.
- Explain the procedure to the child.
- Place the ice cube on a part of the child’s body that is not affected by the epidural e.g. the patient’s forehead or hand and ask if it feels cold.
- Next, place the ice cube below the level of the wound area and work upwards, placing the ice cube at each dermatomal level and on both sides of the body, thus checking that the block is bilateral. (This can also be done on the patients back).
- When the child feels the ice as cold (the same as when placed on their forehead) it is usually a good indication of how far the block has spread. Using the body chart on the epidural laminated guidelines for reference, you will be able to determine the dermatomal level.
- If the child feels the cold stimulus all over the area that is being tested and the child’s pain is controlled do not be alarmed. This occasionally occurs when weak local anaesthetic solutions are used which do not have an effect on the thermo receptors.
Measuring motor block
Epidural infusions used for post-operative pain relief should not cause the patients legs to become weak. The motor nerves are not normally affected by the weak solution of local anaesthetic used but there may be residual motor block if the patient has had a recent top-up in theatre/recovery but this should resolve within 2-4 hours. Patients in bilateral leg cast should be able to wiggle their toes without problem.
This is a side effect that must be acted upon and treated.
- All patients must have their motor block score performed and recorded at the same time as their vital sign observations.
- If the motor block is 2 or 3, the epidural must be temporarily stopped and the Acute Pain Nurse or the Anaesthetist contacted.
Motor Block Score
0 = Full movement
1 = Inability to raise extended leg but able to bend knee
2 = Inability to bend knee but able to flex ankle
3 = No movement
Changing an epidural bag
Equipment
- Epidural prescription sheet
- 200ml bag of 0.125% levobupivacaine.
Procedure
1. Needs to be carried out by registered nurses, one of whom are trained and competent in the administration of medicines by the intravenous Route. Also who has completed Raigmore Hospital training programme in the management of epidural analgesia and the preparation of epidural infusion bags.
2. Check the bag of 0.125% levobupivacaine as follows:
- Check that the bag is intact. Inspect in good light for punctures, discolouration, haziness and crystalline or other particles.
- Date of expiry.
3. Wash hands apply gloves and apron.
4. Ensure that the correct child has been identified.
5. Stop the epidural pump
6. Remove the exhausted bag of levobupivacaine and connect the epidural giving set to the fresh bag.
7. Enter the change programme on pump and press “new container” no 1 in this programme. Review the epidural programme on pump and ensure it corresponds with the epidural prescription sheet.
8. Complete the “refill” section of the epidural prescription sheet.