Bilious vomiting (Management of term babies presenting with bilious vomiting)

Background
Due to bile entering the intestine in the second part of the duodenum, intestinal obstruction distal to the level of the ampulla of Vater can result in bile in the vomit or gastric aspirate¹.
A term baby who presents with bile stained (GREEN) vomiting should be considered to have a possible diagnosis of malrotation until proven otherwise. This condition is associated with considerable morbidity and therefore rapid diagnosis is essential to prevent catastrophic ischaemia occurring.
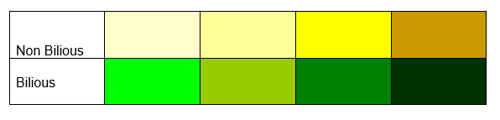
There can be a huge amount of variation in newborns when assessing the colour of their vomit and whether this is bilious or not, as demonstrated below. However bile in the vomit is green not yellow².
If a baby presents with a bilious vomit this must be treated as a time critical case until an upper GI contrast study can confirm or exclude the diagnosis of an abnormality.
Management
Following presentation of a bilious vomit
· Examine the baby in the presence of the parents
· Discuss the baby with a senior in NNU and arrange for the baby to be admitted to SCBU
· Provide the parents with a full explanation as to why the baby is being admitted to SCBU, including the reasons why bilious vomiting causes concern. If you feel you are not the best person to offer this information please contact a senior in NNU to have this discussion.
Following admission to SCBU
· Contact surgical registrar on bleep 9103 and refer the baby providing a thorough handover
· Contact the SE Scotland neonatal transport team
· Commence monitoring on baby; HR, SpO2 and admission temperature
· Site a large bore gastric tube (size 8 or 10fg) depending on the size of the baby) to decompress the stomach and then leave the gastric tube on free drainage
· Obtain IV access with admission bloods if required and a gas to assess acid base status
· Commence maintenance fluids appropriate for baby’s age in postnatal days
· Consider the administration of additional volume in the presence of large gastric losses – may or may not be associated with electrolyte imbalance, acidosis on blood gas or clinical concerns relating to hypovalaemia
· Write a referral letter to the surgical team outlining the situation, background and current management
· If there are other concerns with the baby then these must be managed appropriately, for example respiratory/infection concerns
There is no need for the baby to have an abdominal film prior to transfer to RHSC unless the surgical team request this for alternative reasons
Following return to SCBU in the presence of a normal contrast study
· In the absence of any other concerns there is no need for the baby to remain in SCBU and they should return to their parents to continue with establishment of oral feeding
· PIV and NGT should be removed
· A discharge summary and examination of the newborn should be completed prior to discharge back to the postnatal ward
· If the parents were unable to attend RHSC for the imaging then they should be given a full update at this time
· If there are ongoing concerns with baby and the baby is not fit for discharge these should be managed appropriately following their return
References
1. Walker et al (2006) Colour of bile vomiting in intestinal obstruction in the newborn: questionnaire study BMJ, doi:10/1136/bmj.38859.614352.55
2. Abdhelrim H and Eaton P (2014) Recognition of bile colour in neonates. Archives of Disease in Childhood, doi:10.1136/archdischild-2014-306237.109
