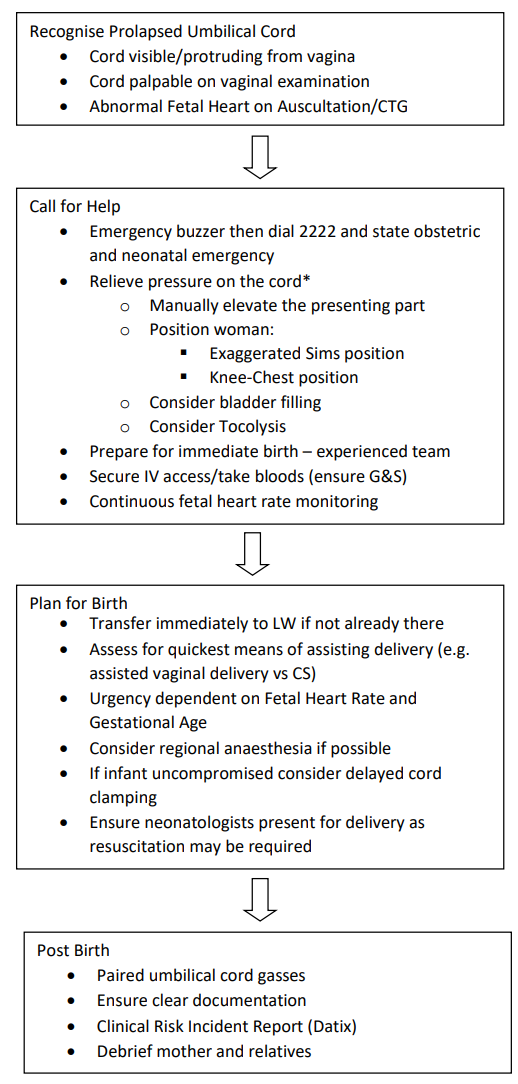
Umbilical Cord Prolapse = a loop of cord below the presenting part with ruptured membranes whether visible or felt on examination
Umbilical Cord Presentation = a loop of cord below the presenting part with intact membranes.
In practical terms acute management is identical and should be immediate.